Accountable Care Services
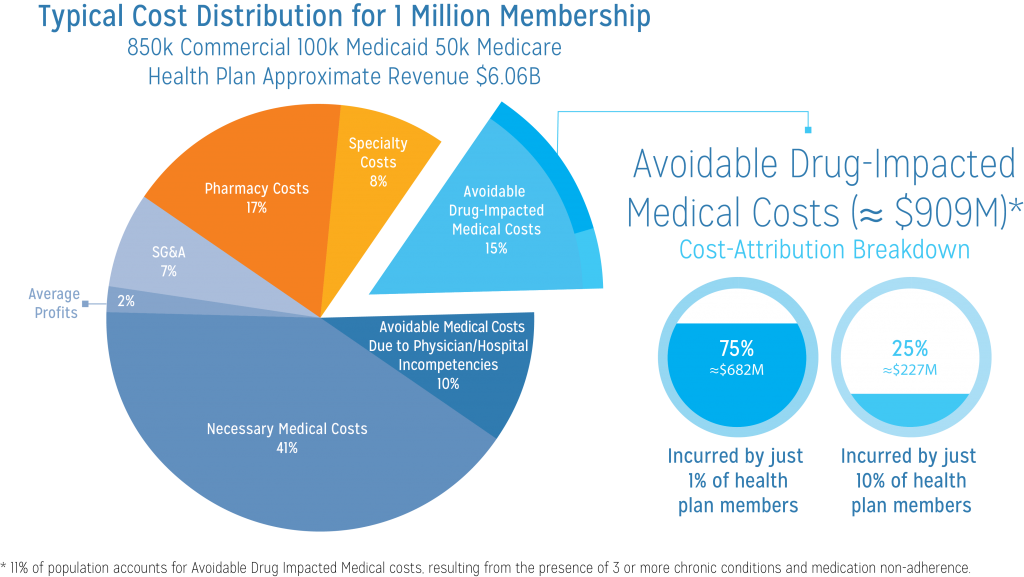
As you may know, 25 to 30% of overall medical costs are unnecessary and avoidable. Approximately half of these avoidable medical costs are due to physician and hospital overuse, abuse, misuse and incompetence, while the other half are classified as avoidable drug-impacted medical costs. These avoidable drug-impacted medical costs include unnecessary ER visits, hospital admissions and readmissions, and rapid patient movement to higher risk bands. These costs come about as a result of adverse drug events, duplicate therapies, poor adherence, absence of personalized care-plan driven vital sign monitoring, lack of actionable intelligence driven timely care coordination, and lack of social interaction for those patients who are depressed, lonely and without family support.
Today, avoidable drug-impacted medical costs account for approximately $350 billion of overall medical costs.
Of these costs, 75% are incurred by just 2-5% of the population. This population constitutes the most unmanaged portion of managed care. Today, health plans, PBMs, doctors, and patients are largely neglecting these costs. This presents an immense opportunity for cost savings.
These costs can be significantly reduced through an accountable drug benefit and care management program.
Aria-Powered Accountable Care Services from nirvanaHealth provides a comprehensive solution that enables collaboration amongst care continuum stakeholders to transform cost into shared savings for all parties—the payer, provider, patient, and nirvanaHealth.
We reduce avoidable drug-impacted medical costs in 6 steps:
STEP 1.
Risk Stratification Using Advanced Clinical Clusters
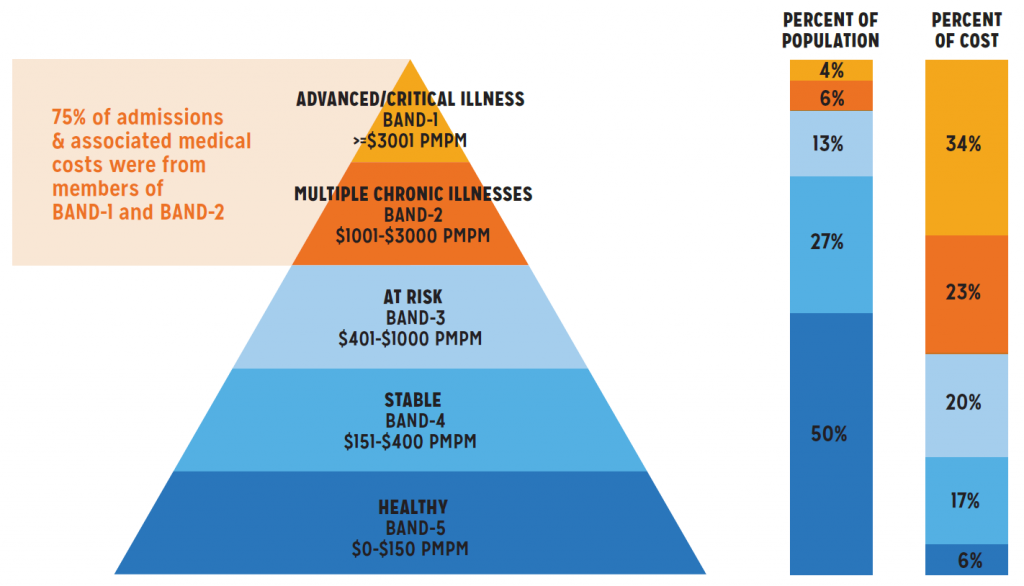
nirvanaHealth uses historical claims data to identify and quantify Avoidable Drug-Impacted Medical Costs and to stratify members based upon risk levels using advanced clinical clusters. Based upon extensive analysis, nirvanaHealth has found that about 10% of the total population can be classified as Advanced Critical Illness and Multiple Chronic Illness patients (Figure 1). This population is responsible for 75% of hospital admissions and 57% of total healthcare costs.
Our Aria platform integrates and analyzes members’ medical, pharmacy, and lab information to create a comprehensive member profile. Proprietary algorithms are applied to map each member to an Advanced Clinical Cluster along with members who share a similar age, gender, socioeconomic, and clinical profile. The impact of medication non-adherence on future medical costs is calculated for each cluster. Members are then stratified based on their risk levels and potential cost savings and are assigned to an appropriate care level. nirvanaHealth offers a three-tiered solution to address the specific needs of chronic care members. Each tiered solution increases in complexity based upon the level of care required by individual members in the corresponding risk band.
Advanced Clinical Clusters Methodology
Advanced Clinical Clusters are leveraged to effectively group members who have similar health profiles. This approach facilitates creating automated, custom care plans, and managing patients who require specific, targeted needs from nirvanaHealth’s care advisors. Furthermore, these clusters allow nirvanaHealth to evaluate member adherence to drug regimens and care plans. Savings opportunities can then be computed for members within each cluster.
- Identify members with a multi-year continuous enrollment
- Integrate medical, pharmacy, and lab claims to build member level clinical and cost history
- Assign medication adherence flag (Y or N) to this distinct population of patients
- Assign chronic condition flag from the CMS identified chronic conditions
- Identify members who have multiple chronic conditions
- Apply proprietary algorithms to build Advanced Clinical Clusters within the member population
- Segment Advanced Clinical Clusters into adherent and non-adherent segments for cost comparison
- Identify Advanced Clinical Clusters with highest per member adherence impact on total costs (medical and pharmacy)
- Compute the potential reduction of Avoidable Drug-Impacted Medical Costs for each identified member within the Advanced Clinical Clusters
STEP 2.
Comprehensive Medication Review & Personalized Care Plan Derivation
During this step, when an eligible member visits their primary care physician, a personalized medication list and customized care management plan is created. The primary care physician reviews both the medication list and care plan, and obtains the member’s consent to begin the care regimen across the following components
Physician-Led Comprehensive Medication Review (CMR)
When a prescriber is writing a new prescription, or renewing an existing prescription, the prescriber will be alerted in his/her own workflow (EMR/PM/e-Prescription software) with both existing Adverse Drug Events and additional events due to new/current prescriptions. The prescriber will also be alerted with patient Medication Therapy Management (MTM) eligibility and the opportunity to conduct a comprehensive medication review (using CMS and plan rules) and reconciliation. The prescriber will also be alerted to correct all ADEs in an organized manner and will have the ability to quickly issue a new Medication Action Plan (MAP) with essential medications to improve patient’s overall quality of life. Along with medication reconciliation, this service also includes the creation of a Personal Medication List (PML).
Duplicate Therapy Reduction
Due to the fragmented systems that are pervasive in healthcare today, a patient’s laboratory, medical, and pharmacy data are rarely integrated in a single system. As a result, different specialists (often unknowingly) prescribe overlapping medication therapies for a single patient. A core component of the medication reconciliation process accomplished through the physician-led CMR is the identification and elimination of all duplicate therapies through our Aria platform. Removal of these duplicate therapies allows the primary care physician to improve both the quality and cost of the patient’s medication regimen, right at the point of care.
Adverse Drug Event (ADE) Reduction
The core objective of the medication reconciliation process, accomplished through the physician-led CMR, is the reduction of Adverse Drug Events (ADEs). This step identifies drugs that are causing more harm than good to the patient and eliminates them from the member’s medication list. Our Accountable Care Services identify all adverse drug events and communicates these to the patient. A corrective action plan is then created, captured, and implemented. The prescriber will now also have the ability to quickly issue a new Medication Action Plan and Personal Medication List with essential medications to improve patient’s overall quality of life. Patients are educated about their new medications and methods of improving their drug regimen.
Customized SmartCarePlan™ Creation
Aria’s proprietary algorithms analyze the age, gender, clinical, and socioeconomic data of at-risk members to provide a customized baseline care plan. After a member is assigned to a specific Advanced Clinical Cluster, a SmartCarePlan™ is shared with all stakeholders including care advisors, primary care physicians, family caregivers, and the member himself via nirvanaHealth’s Aria platform. This ensures uninterrupted care, even when the patient is at home. SmartCarePlan™ includes customized medication lists, vital reminders, exercise routines, nutrition coaching, and preventative care scheduling, including gaps in care and continuity of care measures. These tools help improve compliance management protocols as well as provide alerts at thresholds optimized for the individual member’s condition.
STEP 3.
SmartAdherence™ Management
nirvanaHealth’s unique value proposition for adherence includes delivery of an intelligent, prefilled, disposable SmartTray™. After drug utilization review at the point of care, nirvanaHealth’s SmartTray™ is appropriately filled with the patient’s medications and paired with the nirvanaSmart™ device.
SmartTray™ Delivery Management
nirvanaHealth provides a fully automated, comprehensive medication adherence management solution that engages all care stakeholders at every touch point in the care continuum. SmartTray™ delivery management includes the following actions:
- Outreach and educate: After being enrolled by their Primary Care Physicians, nirvanaHealth care advisors proactively reach out to eligible patients for comprehensive pre-program patient education.
- Organize: During this stage, nirvanaHealth aggregates medications through a disposable SmartTray™, providing convenience to patients and ensuring that all medications are organized appropriately.
- Install: During this stage, a Bluetooth-enabled and patented nirvanaSmart™ is shipped to and installed in the patient’s residence. This device is wirelessly connected to the Aria platform. nirvanaSmart™ also monitors vital signs from Bluetooth-enabled measuring equipment such blood pressure monitors, glucometers, weighing scales, thermometers, and pulse oximeters. It collects, consolidates, and transmits the member’s adherence and vital signs data to the Aria platform in real time.
- Dispense: After installation, nirvanaHealth aggregates and delivers all medications to the patient’s home on a weekly or bi-weekly basis from a centralized location using our electronic prefilled disposable pill trays.
Comprehensive Adherence Monitoring
Following successful installation, the nirvanaSmart™ will monitor and notify the patient with voice alerts when it is time to take their medication and will further remind the patient with to-dos to capture vital sign measurements. Based upon the patient’s disease states, medications, and vital sign values, nirvanaSmart™ appropriately alerts patients for care coordination. It also pushes real-time alerts to caregivers (such as family members) via their smart phones, and to nirvanaHealth care advisors and care/case managers at the health plan within their respective workflows. On an ongoing basis, the Aria platform analyzes patient adherence and automatically generates alerts that are tracked by care advisors who are able to reach out to non-adherent patients. Dedicated nirvanaHealth care advisors are able to engage with members to build a social connection and to collect vital well-being information not otherwise available.
STEP 4.
SmartHomeCarePlan™ Management
Identified members not only undergo comprehensive adherence monitoring, but are also provided with complete Bluetooth-enabled vital signs monitoring devices, dynamic care plan management, and timely care coordination. With these comprehensive technology-driven services, a patient’s clinical team is empowered provide a high level of care at right at the patient’s home, as if under direct observation.
Vital Signs Monitoring
nirvanaSmart™ seamlessly pairs with and integrates data from Bluetooth-enabled monitoring devices that are included with our Accountable Care services. Based upon the patient-specific care plan, these devices monitor the patient’s blood pressure, weight, temperature, blood glucose levels, pulse, and oxygen saturation at appropriate intervals. Measurements obtained via these devices are then compared to patient-specific threshold values.
Dynamic Care Plan Management & Smart Care Coordination
In real time, nirvanaHealth integrates vital measurements and updates clinical/lab information to dynamically adapt a patient’s baseline care plan. This newly derived care plan, comprising of “updated” threshold measures such as blood pressure and weight, triggers actionable intelligence alerts that are pushed directly into the workflows of nirvanaHealth’s care coordination team members. These alerts can also help nirvanaHealth and the plan sponsors to identify the precursors to major health events and enable the care coordination team to take timely corrective actions.
STEP 5.
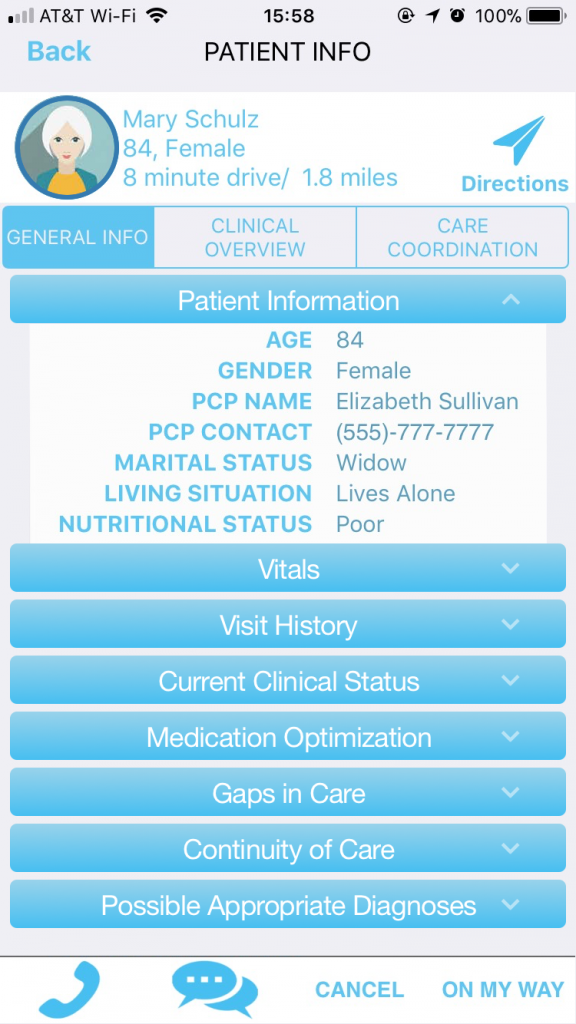
SmartHomeCarePlan™ Delivery Management
When a member’s vitals cross pre-defined thresholds, an alert is generated, and a designated nirvanaHealth care advisor will immediately review the member’s clinical status. Care advisors then contact the member to address all concerns. If appropriate for the member’s condition, the care advisor will prompt a home visit from nirvanaHealth’s physician network. Network physicians within a 10-mile radius of the member’s location will be alerted of the patient’s status and their need for a home visit via the nirvanaSmart™ mobile application. Any nirvanaHealth network physician will have access to the member’s location, complaints, and clinical status and may accept the visit. During the home visit, the physician will address the patient’s current clinical problems to prevent an unnecessary ER visit or hospitalization. In addition, the physician will also be informed of opportunities available to optimize medications, perform comprehensive gaps in care measures, and other value-added care coordination activities.
nirvanaSmart™ Mobile App
Through nirvanaSmart™, any changes in clinical condition, medications, and other care coordination activities performed by the visiting doctor will be updated in the member’s medical record. This information will then be shared with all stakeholders across the care continuum, including family members, caregivers, physicians, and health plan case managers, to ensure uninterrupted member care.
STEP 6.
Risk & Shared Savings Management
As part of implementation activities, key performance metrics, success criteria, and program monitoring timelines are defined. All computations are clearly documented before the program is initiated to ensure consistency of measurements. These metrics will be defined and included in more detail in the master services contract/agreement. Typical stakeholders include participating members, plan sponsors, prescribers (primary care physician and network physicians), and nirvanaHealth, all of whom will sign individual agreements.
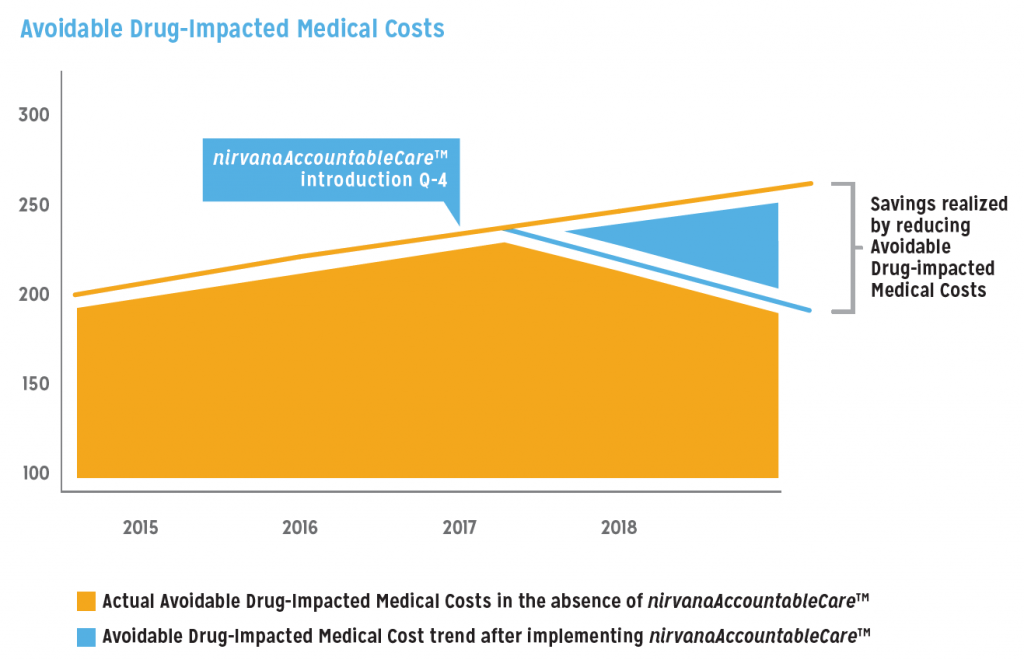
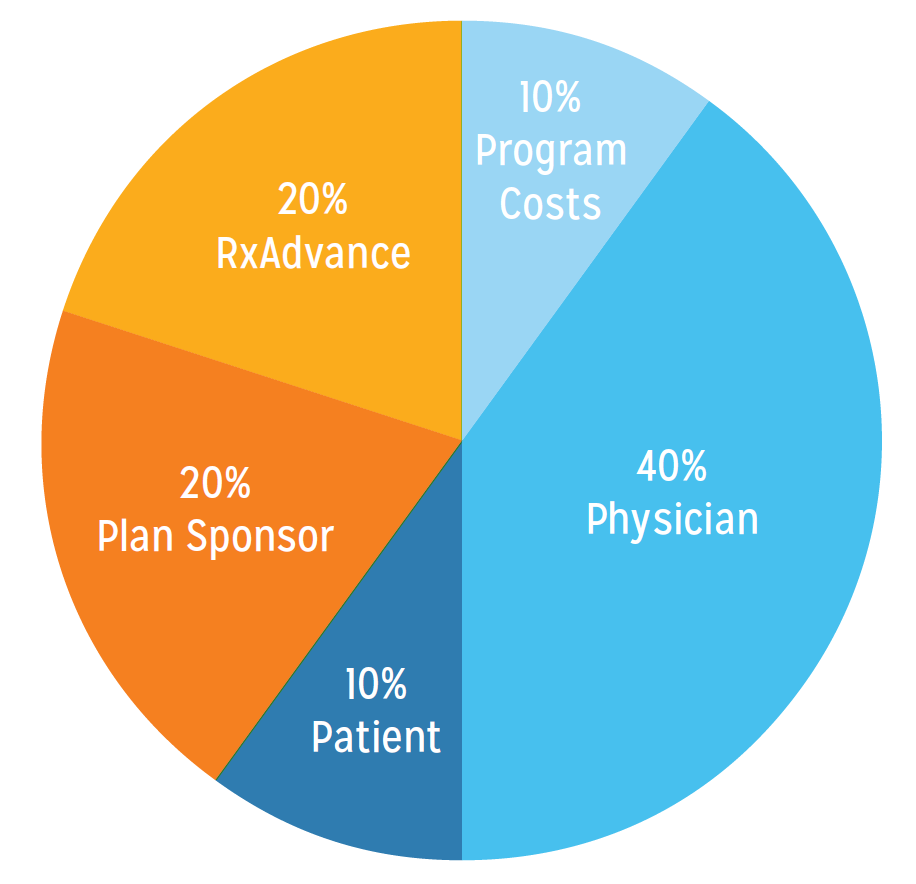
nirvanaHealth will fund the cost to run the program in exchange for the opportunity to capture a portion of the savings that result from reduced Avoidable Drug-Impacted Medical Costs (Figure 2). nirvanaHealth will utilize its resources to implement, monitor, and deliver financial outcomes. However, nirvanaHealth seeks support from the client’s clinicians, case managers, and supporting staff in facilitating communications with patients and providers surrounding this new program to improve patient quality of life. These communications will be conducted through electronic communications and provider workshops, which will derive incentive programs for prescribers and patients. Successful implementation heavily relies on the support of the client, as the client fosters the relationship with the members and prescribers.
Shared Savings
The program in its entirety is continually monitored for effectiveness and to identify any opportunity for appropriate recalibrations in order to achieve superior outcomes and savings. nirvanaHealth will work with the client to compute cost reduction results and to mitigate clinical risks. Based upon the results accomplished and the cost savings achieved, the resulting reward will be shared between the client and nirvanaHealth in accordance with predefined contractual terms.